APICAL PROLAPSE (UTERINE OR VAGINAL VAULT PROLAPSE)
WHAT IS UTERINE PROLAPSE?
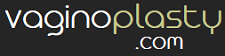
Uterine prolapse is when the uterus or womb prolapses into or out of the vagina. Pelvic floor support is made up of 3 compartments or areas in the vagina and pelvis that may fall or prolapse. The anterior vaginal wall (bladder support), the posterior vaginal wall (rectum support) and the apex or top of the vagina (upper 1/3 of the vagina) which includes the support of the uterus. The uterosacral and cardinal ligament complex provide the support to the uterus and upper 1/3 of the vagina. If these ligaments get stretched or torn, during childbirth or aging, this causes the uterus to drop or prolapse. Typically, the uterus does NOT just fall by itself, other compartments are usually involved as well including the bladder and or rectum. Therefore, it is vital to have an exam by an experienced Urogynecologist, Gynecologist or Urologist that is trained in the diagnosis of pelvic organ prolapse. The diagnosis is made on pelvic exam both in the lying and standing position. If the prolapse is not seen with the patient laying down, then an exam should also be done in the standing position.
Symptoms of Uterine prolapse
Symptoms of uterine prolapse are very similar to cystocele or rectocele including pressure, pain or discomfort in the vagina and/or pelvis, low back discomfort, urinary urgency/frequency, urinary leakage, pain with intercourse and bowel dysfunction in the form of difficulty in emptying the rectum during bowel movements. The ligaments that support the uterus (ie the uterosacral ligaments) originate in the sacral spine area and therefore if the uterus is falling, these ligaments are stretched or torn and a woman may suffer from low back discomfort from the prolapse. Some women also have pain in the lower part of the abdomen, especially at the end of the day if they have been on their feet a lot during the day secondary to the fact that the prolapse can worsen through the day and cause more symptoms at the end of the day. Some women find relief by getting off their feet or laying down, which helps take the pressure off of the pelvic floor.
Treatment options for Uterine Prolapse
If the uterine prolapse is mild and not causing any symptoms, it can just be monitored and observed until it starts causing symptoms. Conservative or non-surgical therapy includes pelvic floor physical therapy which includes specialized training in Kegel or pelvic floor muscle exercises, electric stimulation, biofeedback, bowel movement strategy and other treatment modalities that can help reduce symptoms, however will not cure prolapse. Another non-surgical option is a pessary. A pessary is a rubber or silicone donut shaped device that is placed inside of the vagina to support the prolapse. It must be big enough to stay in the vagina and support the prolapse, but not too big to cause discomfort. Most women use pessaries as a temporary solution to the prolapse or if their health is too poor for surgical correction.
Surgical treatment options for Uterine Prolapse
Depending on the degree or stage of prolapse and what other prolapse may be present (it is very rare to just have a uterine prolapse by itself, ie typically there are other organs falling at same time such as the uterus or bladder that must be treated at same time), surgical options vary by the experience of the surgeon. A surgeon should be experienced and an expert in Urogynecology and Female Urology surgery to be able to identify other defects in pelvic support and then utilize the appropriate surgical treatments to achieve the best cure rate for the patient. Cure rates are dependent not just on the treatment of the uterine prolapse, but also support at the apex of the vagina, ie treating vault prolapse or uterine prolapse at the same time.
Uterine Suspension versus Hysterectomy
Traditionally, hysterectomy or removal of the uterus was always recommended at the time of surgery for uterine prolapse. This was not secondary to the fact that there was something pathologically wrong with the uterus itself, it had more to do with the fact that uterine suspension procedures in the past did not work or had very low cure rates. Just because the uterus is falling and dropping doesn’t mean there is something wrong with it, however the uterus was considered to be in the way of repairing the support to the top of the vagina, therefore it was removed and then the vaginal vault was then suspended. More recently, however, techniques have been developed to overcome these issues and successfully suspend the uterus and top of the vagina, without having to do a hysterectomy in select patients that would like to save their uterus.
Uterine Preservation/Sparing Options- Uterine Suspension
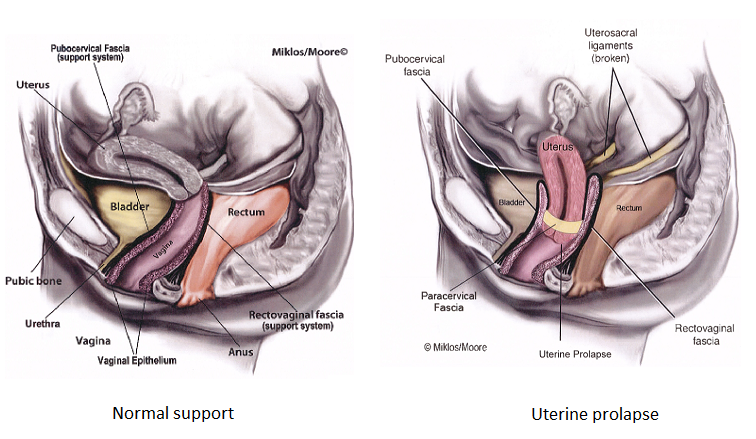
In women that would like to preserve their uterus and not undergo hysterectomy, Uterine suspension surgery is an option. Traditional suspension using the ligaments that support the uterus, ie the round ligaments and the uterosacral ligaments, have high failure rates in women with moderate or severe prolapse and therefore is not recommended in these situations. In women with moderate to severe uterine prolapse a Mesh Hysteropexy (or mesh sacrohysteropexy) which is a Mesh suspension of the uterus is now the current recommendation for women with uterine prolapse that would like to preserve their uterus. The procedure has cure rates well over 90% and is an ideal option for women that are younger or just do not want to have their uterus removed for one reason or another. However, if the uterus has abnormalities such as large fibroids or the woman has any history of pre-cancerous lesions of the uterus or cervix, she may not be a good candidate to keep the uterus in place. For complete details of Uterine Suspension procedures please CLICK HERE
Removal of Uterus (Hysterectomy) with Suspension of the Top of the Vagina
The more traditional approach to Uterine Prolapse is removal of the uterus (hysterectomy) with suspension of the top of the vagina via an abdominal or vaginal approach using the patient’s own ligaments (uterosacral or sacrospinous ligament suspension) or mesh (Sacralcopopexy). As stated above, the more traditional approach is to remove the uterus at time of surgery and then suspend the apex or top of the vagina. Many times, with uterine prolapse, the uterus is in the way of achieving a good suspension of the top of the vagina. There may be hernias (also known as enterocele) in front of or behind the uterus and these are difficult to repair with the uterus in place. Therefore the uterus is removed, any hernia (enterocele) at the top of the vagina is repaired and then the apex of the vagina suspended with either the patient’s own ligaments or with the use of mesh.
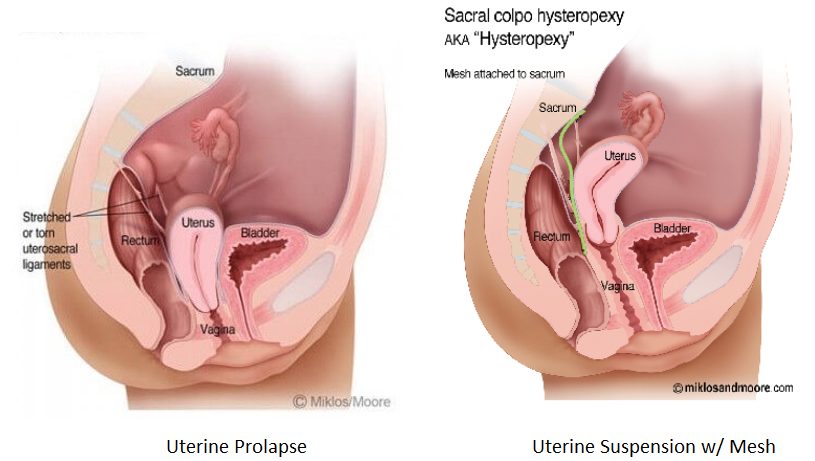
The abdominal approach to hysterectomy and vault suspension can be achieved through an open abdominal incision (called a laparotomy) or through a minimally invasive approach with laparoscopic or robotic surgery. Most surgeons utilize these more minimally invasive approaches to complete the hysterectomy and vault suspension as there is no large incision to heal, recovery is faster, blood loss typically less, infection rates lower and hospital stay is usually only 24 hours compared to 3-4 days. Recovery at home with laparoscopic/robotic surgery is typically in the range of 1-2 weeks versus 4-6 weeks with open incision surgery. Laparoscopic surgery is completed by placing a camera through a small incision hidden in the belly button, and then using several other tiny incisions to work through. Laparoscopic surgery is done with the surgeons own hands whereas Robotic surgery, the same incisions are used however the arms of the robot are controlled by the surgeon sitting at a console away from the patient. It is also referred to Robotic-assisted Laparoscopic surgery.
Hysterectomy
Hysterectomy is traditionally completed at the time of uterine prolapse surgery. Hysterectomy means removal of the uterus or the womb only. The uterus is an end organ, meaning it does NOT produce any hormones (such as estrogen or progesterone), its only job is to maintain and carry a pregnancy. Each month the OVARIES produce hormones working in conjunction with the pituitary gland and the brain to get the lining of the uterus ready for a pregnancy. If a pregnancy does not occur, the woman then sluffs this lining and the woman has her period or menses. Unless the woman is over 60-65, typically the ovaries are left in place and are NOT removed at the time of hysterectomy, therefore the woman’s hormone levels should not change. Many women think of hysterectomy as an automatic entrance into menopause, and unless the ovaries are removed, this is not true at all. The hormone levels should not change if the ovaries are left in place. Studies have shown that sexual function does not change, nor is affected by hysterectomy. Hysterectomy does not cause prolapse either, ie the prolapse is already present, however the vaginal vault must be suspended after the hysterectomy as the prolapse is not cured by hysterectomy alone! The fallopian tubes should be removed at time of hysterectomy as they have been shown to be a cause of cancer later in life. The ovaries should be removed at time of surgery in post-menopausal women over 65 years old or in younger women that have a high risk of ovarian cancer, otherwise the ovaries should be left in place at the time of the surgery.
Women with enlarged uteri secondary to fibroids or adenomyosis, pain with intercourse secondary to their uterus, irregular or heavy menstrual bleeding that is not able to be controlled with hormones or other methods, or women with a history of cancerous or pre-cancerous cells should not consider uterine preservation and should undergo hysterectomy at time of uterine prolapse surgery.
Vaginal Approach to Hysterectomy with Vault Suspension
Hysterectomy or removal of the uterus may be completed through the vagina in certain cases. The advantage of this approach is that it is minimally invasive and avoids having to make any incisions in the abdomen. Surgeons that prefer to complete prolapse surgery completely through a vaginal approach, many times will elect to complete the hysterectomy through the vagina as well. Hysterectomy is typically the first procedure completed prior to vault suspension and repair of bladder or rectal prolapse. The surgery may be completed under general anesthesia and in certain cases, may be completed under spinal or regional anesthesia. An incision is made around the cervix, the bladder is dissected away from the uterus and clamps are used to seal blood vessels and the uterus is then delivered through the vagina. The vaginal vault suspension is completed with either the uterosacral ligaments or the sacrospinous ligament and the vaginal cuff closed with sutures that dissolve over a period of time. Other prolapse repairs (such as Cystocele or Rectocele) and incontinence procedures, such as a (sling), can then be completed all through the vagina.
Abdominal/Laparoscopic/Robootic Approach to Hysterectomy with Vault Suspension
Hysterectomy may also be completed through the abdomen through a large incision called a laparotomy, however these days is most commonly completed through a minimally invasive laparoscopic or robotic approach. With laparoscopic/robotic surgery, the surgery is completed through mini- incisions in the abdomen and the uterus delivered through the vagina. The surgery is completed with a camera placed through a tiny incision in the belly button and the image is projected onto large TV screens or monitors that magnifies the images for the surgeon. Once the uterus is removed then the top of the vagina or the vaginal vault suspension may be completed via Uterosacral vault suspension (patients own ligaments) or mesh with sacralcolpopexy. For more details on the Vaginal Vault suspension procedure please click here.
Post-operative course and recovery following Hysterectomy and Vault Suspension
With vaginal or Laparoscopic/robotic surgery recovery is much easier and faster than with an open abdominal incision. With a minimally invasive approach, such as completing the surgery through the vagina only or with mini-incisions in the abdomen with laparoscopic/robotic surgery, hospital stay is usually 24 hours or less and recovery at home is typically in the range of 1-2 weeks. Many patients may return to work in as little as a week if their job is not strenuous or require heavy lifting. Most surgeons place patients on activity restrictions (ie avoiding vigorous exercise, heavy lifting) for a period of 6-8 weeks. The most important thing in the healing process is to avoid lifting or straining a lot into the pelvis. This is avoided by avoiding any lifting, pushing or pulling that causes straining into the pelvis. Of course, you have to strain a little getting out of bed, having a bowel movement etc….but the important thing is to try to avoid heavy straining. Most surgeons place patients on a bowel regimen following surgery including stool softeners and/or laxatives to avoid constipation and straining with bowel movements. Sexual function is restricted for 6-8 weeks depending on the procedures completed.
Recovery is much longer with an open abdominal surgery through a large incision as hospital stays are in the range of 3-4 days and recovery at home is usually in the range of 4-6 weeks compared to 1-2 weeks with vaginal or laparoscopic approach.
Cure rates and Risks of Hysterectomy with vault suspension
Cure rates for are in the range of 80-90% depending on the type of vault suspension completed (for more details on vault suspension procedures click here). As with any surgery, there are risks, however hysterectomy is a relatively low risk surgical procedure. Risks during surgery include injury to the bladder or the ureters (tubes from the kidneys to the bladder) or injury to the bowel. Risk of bladder, ureter or bowel injury is less than 1%. If there is an injury to one of these organs there is a risk of a fistula, which is a hole or connection from the bladder or the bowel to the vagina and would result in leakage of urine or stool into the vagina. Risks of a fistula following hysterectomy are also very low and in the range of 1% or less. Bleeding requiring transfusion is also a very low risk, however if the uterus is enlarged secondary to fibroids this risk does increase. Infection following hysterectomy is a risk given the fact the vagina is not a sterile environment, ie there a lot of bacteria in the vagina (like the mouth) and therefore there is a risk of infection following hysterectomy in the range of 1%. Antibiotics are given intravenously at the time of surgery to minimize this risk. Other risks of hysterectomy with vault suspension are worsening urinary urgency/frequency or leakage (1-2%), pain with intercourse (1-3%) , pain in the buttocks or pelvis that does not resolve (ie nerve irritation or injury) <1% and hematoma or infection (<1%).