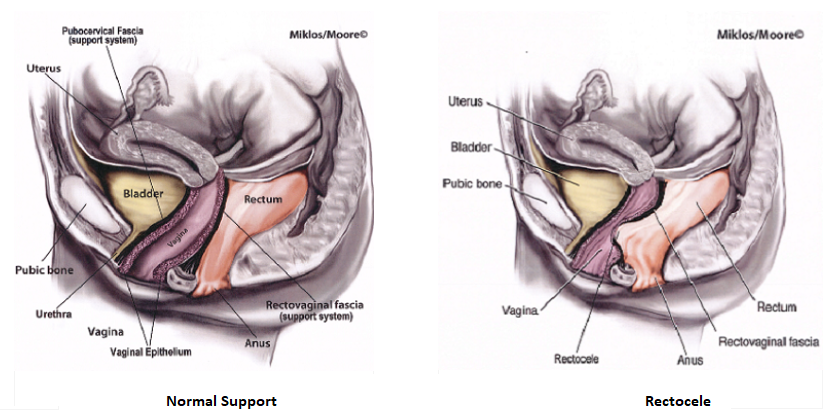
| What is a Rectocele? A rectocele is a form of pelvic organ prolapse in women and may also be called Posterior Vaginal Wall Prolapse secondary to the fact that the posterior or back wall of the vagina supports the rectum in the female. A rectocele is a very common form of pelvic organ prolapse in women. The posterior vaginal wall forms the floor of the vagina and the ceiling over the rectum and gives the rectume support during pressure events, like bearing down to have a bowel movement. The posterior vaginal wall goes from one side of the pelvis to the other and is attached to the pelvic floor muscles on each side. The posterior wall is also responsible for the caliber or diameter of the vaginal canal. Damage to the connective tissue of the posterior vaginal wall from vaginal childbirth and/or aging is thought to be the cause of a Rectocele. Rectocele’s can also be caused by chronic constipation and/or straining. The supportive tissue or fascia in the posterior wall can can actually tear away from its connection to the pelvic muscles or the wall can stretch out, both causing the rectum to bulge up into or out of the vagina.
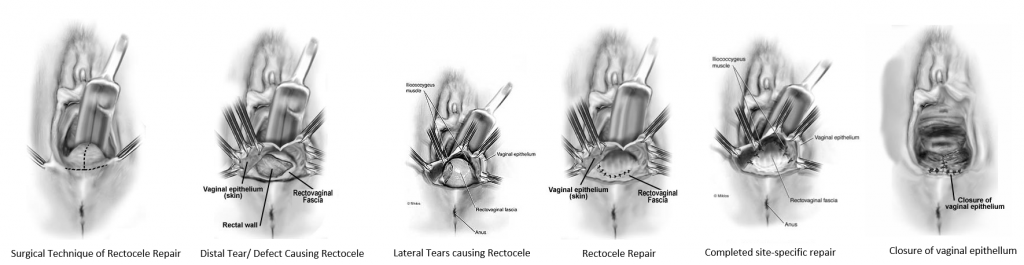
Symptoms of a rectocele include feeling a bulge inside or coming out of the vagina. This can cause pressure or discomfort for the women. Some women complain of pain with intercourse secondary to the rectocele. A rectocele can also cause bowel dysfunction in the form of difficulty evacuating the rectum with a bowel movement. This will cause the woman to strain more to try to have a bowel movement as she feels like the stool is stuck or she cant get it out of the rectum. The sensation that the stool is present, however she feels like she cant get it out. This is secondary to the fact the rectum is bulging up or out of the vagina and the stool gets trapped in this bulge. The posterior vaginal wall typically provides the support during straining with a bowel movement to direct the stool out of the anus. If the support is not there, it makes having a bowel movement more difficult. In many cases a woman may actually hold onto the perineum or place a finger in the vagina to push down on the bulge to help have a bowel movement. This is called digitation and what she is doing is providing the support to the floor of the vagina that has been lost with the rectocele, which helps facilitate a bowel movement. Some women may also have mild stool or gas leakage secondary to the rectocele. Treatment for Posterior Vaginal Wall Prolapse / Rectocele If the rectocele prolapse is mild and not causing any symptoms, it can just be monitored and observed until it starts causing symptoms. Conservative or non-surgical therapy includes pelvic floor physical therapy which includes specialized training in Kegel or pelvic floor muscle exercises, electric stimulation, biofeedback, bowel movement strategy and other treatment modalities that can help reduce symptoms, however will not cure prolapse. Another non-surgical option is a pessary. A pessary is a rubber or silicone donut shaped device that is placed inside of the vagina to support the prolapse. It must be big enough to stay in the vagina and support the prolapse, but not too big to cause discomfort. Most women use pessaries as a temporary solution to the prolapse or if their health is too poor for surgical correction. Surgical Treatment of Rectocele Depending on the size of the rectocele and what other prolapse may be present (it is very rare to just have a rectocele by itself, ie typically there are other organs falling at same time such as the uterus or bladder that must be treated at same time), surgical options vary by the experience of the surgeon. A surgeon should be experienced and an expert in Urogynecology and Female Urology surgery to be able to identify other defects in pelvic support and then utilize the appropriate surgical treatments to achieve the best cure rate for the patient. Cure rates are dependent not just on the treatment of the cystocele, but also support at the apex of the vagina, ie treating vault prolapse or uterine prolapse at the same time. Vaginal approach It has been shown by multiple studies that the most successful approach for surgical treatment of a rectocele is through a vaginal approach which is called a Posterior Repair. The surgery may be completed under local anesthesia with sedation (monitored anesthesia care), epidural/spinal or with general anesthesia. Local anesthesia is injected into the posterior vaginal wall and an incision is made along the posterior wall. The vaginal wall is then dissected off the underlying rectovaginal fascia (ie the supportive layer that is stretched out or torn) all the way out to the pelvic muscles on each side and up to the top of the vagina. Any tears in the fascia are repaired with sutures and/or the stretched-out fascia is tightened and the bulge reduced with sutures. This results in reducing the bulge of the rectocele and restoring the support of the floor of the vagina. Any stretched out or excess vaginal skin is excised and the vaginal incision is closed. In some cases, a biologic or dermal graft may be used to provide additional support over the repair. Mesh use in the posterior compartment has not been shown to be beneficial and is not recommended at this time. A trans-rectal approach (ie repairing the rectocele through the rectum instead of the the vagina) is not recommended and been shown to have lower cure rates compared to the vaginal approach.
Cure rates and Risks of Surgery Cure rates for are in the range of 80-90%. Symptoms of defacatory dysfunction caused by a rectocele, ie difficulty evacuating the rectum with bowel movements, improve significantly in approximately 70% of women. Global constipation or slow transit constipation, ie constipation that was present prior to the rectocele being present and not caused by the rectocele, will not improve with surgical repair of a rectocele. This type of constipation needs treated non-surgically and is important to treat after rectocele repair as chronic straining will lead to a higher failure rate for the rectocele repair. As with any surgery, there are risks, however repair of a rectocele is a relatively low risk surgical procedure. Risks include injury to the rectum which is very rare and in the range of less than 1% and repaired at the time of surgery if recognized. Fistula formation (ie a connection or tract from the rectum to the vagina and results in stool leakage through the vagina) is very rare and less than 1%. Other risks including bleeding requiring transfusion (<1%), worsening urinary urgency/frequency or leakage (1-2%), pain with intercourse (1-3%) , hematoma or infection (<1%) and breakdown of the incision 1%. Cost of surgery is typically covered by insurance, therefore check with your insurance company regarding deductible, co-pays, etc. |

 What are the symptoms of a rectocele?
What are the symptoms of a rectocele?