Pelvic Organ Prolapse also known as POP occurs when the support of the female organs is compromised or weakened and results in the uterus, bladder or rectum falling into the vagina and/or bulging out of it. Typically, female pelvic organ prolapse results following childbirth and/or the aging process, although there is a genetic component and therefore can occur in women that have not had children or been pregnant. This may occur in women that do chronic heavy lifting (ie in their jobs) or have a chronic cough from asthma or other lung conditions or just have genetically weak support tissues. Prolapse has been known to occur even in young women in the military that are paratroopers and they have never had children! Clearly, they must have had a genetic weak pelvic floor as this is a very rare occurrence. It is thought that over 3 million women in the US and that between 10-25% of women that have children via vaginal birth will suffer from prolapse or incontinence. There are over 200,000 women in the US yearly that have surgery to treat pelvic organ prolapse. It can occur in women as early as in their 20’s and as late as in their 90’s. Surgery for prolapse is one of the most common surgeries that women over 70 undergo.
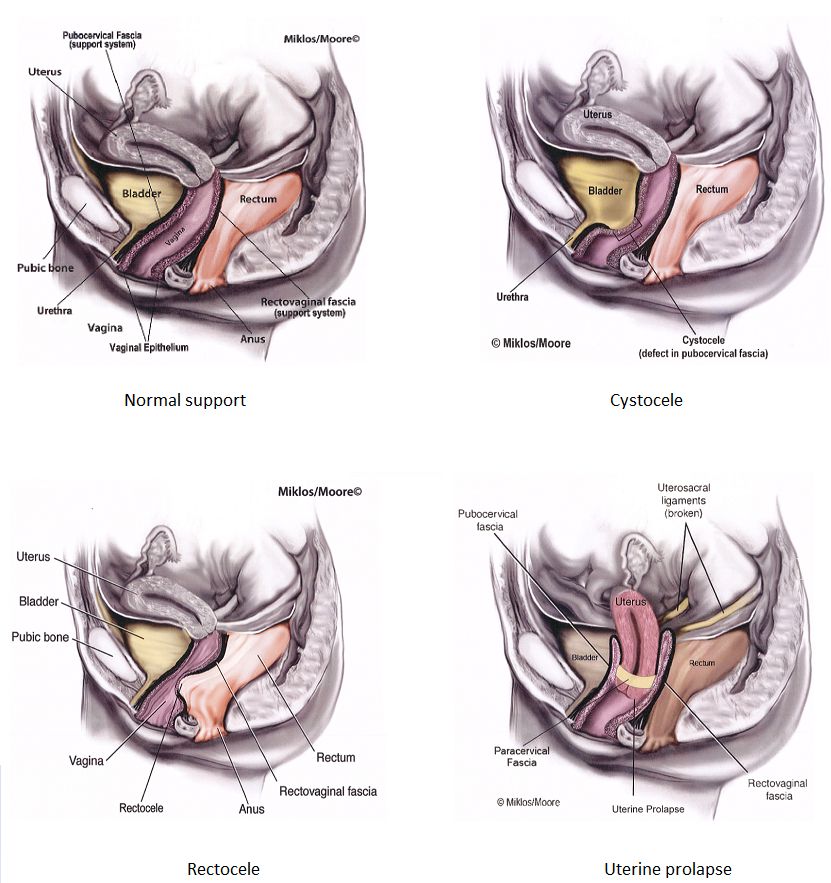
Pelvic organ prolapse may be categorized as a cystocele when the bladder is dropping, a rectocele when the rectum is bulging into or out of the vagina, an enterocele when bowel is bulging into the vagina or uterine prolapse when the uterus is dropping. Typically however, the organs don’t drop individually, they usually come down together. One may be worse than the others but for example, when the bladder is dropping, it usually is pulling the uterus down with it at the same time. Prolapse is also staged or graded from 0 to 4 depending on the extent of the prolapse. Grade/stage 0 means no prolapse at all, 1 and 2 mild/early moderate prolapse, 3 and 4 more extensive and large.
What is the common thread between all of the above?
Meaning, what may be the cause of prolapse of the female organs in a woman?? It seems that childbirth and/or aging or chronic pressure down into the pelvis can cause tears of the support tissues of the vagina and the pelvic muscles that give support to these organs. The vaginal walls actually support the the bladder and the rectum and these walls can tear away from the pelvic floor muscles, also known as the levator ani muscles including the pubococcygeus muscle (ie the PC muscle) and this can cause the bladder or rectum to bulge into the vagina or actually start bulging out of the vagina! It may happen suddenly (many woman all of a sudden may feel something bulging out of their vagina in the shower and are terrified as they have no idea what they are feeling!), or it may happen slowly over time. If the vaginal walls tear away from the muscles that they are attached, it will result in the organs dropping. Or if the walls have a defect or tear in the middle of them, or just become stretched out this will also result in the organs dropping or bulging. Weakening or damage to the pelvic floor muscles themselves can also cause the organs to drop or prolapse.
What are the symptoms of pelvic organ prolapse?
Besides feeling a bulge in the vagina or seeing a bulge coming out of the vagina, prolapse can also cause pressure or discomfort in the vagina. Some women may also experience low back pain or discomfort from the prolapse pulling on the pelvic floor muscles, which originate near the sacrum and also connected to some of the low back muscles. Prolapse may also cause pain with intercourse if the uterus or other organs that are dropping and getting hit by the penis during sex. Prolapse of the bladder, or cystocele may also cause urinary symptoms such as urinary urgency, frequency or urinary leakage. A rectocele can cause bowel symptoms in women such as having a hard time evacuating her stools with her bowel movements or even occasionally can cause leakage of stool or gas.
Is pelvic organ prolapse dangerous?
The answer is no (unless in very rare cases the prolapse gets so severe that the bulge cant be reduced back into the vagina and cause retention of urine and ultimately pressure and damage to the kidney’s themselves).
What are the treatment options for Prolapse?
Mild prolapse or prolapse that is not causing any symptoms does not necessarily need treated, ie it can be treated conservatively without intervention and just monitored. If the prolapse worsens and starts causing symptoms then treatment can be completed at that time. Treatment options include other conservative ones such as pelvic floor physical therapy or a pessary. Pelvic floor physical therapy is completed by licensed physical therapists that specialize in strengthening the pelvic floor muscles. These are also known as “kegel” exercises, however the therapists use other modalities to help you to learn how to do the Kegel exercises properly as well to strengthen the muscles on your own. Pelvic floor therapy or kegel exercisises will not reverse or cure prolapse, however it may help with some of the symptoms. A pessary is a rubber donut of sorts (there is different sizes depending on size of prolapse) that gets placed in the vagina and worn daily to support the dropped organs. The pessary should fit comfortably and may help alleviate some symptoms of prolapse.
Surgery is also an option and the most definitive form of treatment for prolapse. There are many different types of surgeries depending on the extent of the prolapse, the specific type, the patient’s symptoms, the health of the woman, the patient’s desire as type if surgery she may desire, as well as the experience of the surgeon. The surgery can be completed through the vagina only, or an abdominal approach may be utilized either through a large incision or minimally invasively with a laparoscopic or robotic approach. There are surgeries that utilize the patient’s own tissue or sometimes grafts such as mesh are recommended. Hysterectomy is recommended in many situations, however uterine preservation surgery is becoming more common now as well. For complete details of surgical options for the different types of prolapse, please review that particular section.
