Hysteropexy (aka the sacrocolpopexy with the uterus in place or sacrocolpohysteropexy) is a uterine suspension or uterine preservation surgical procedure to restore support of the uterus after a patient has been diagnosed with uterine prolapse (ie descension). Hystero means uterus and pexy means support. Hysteropexy should not be confused with the term hysterectomy (hystero = uterus, ectomy = removal) which means to remove the uterus.
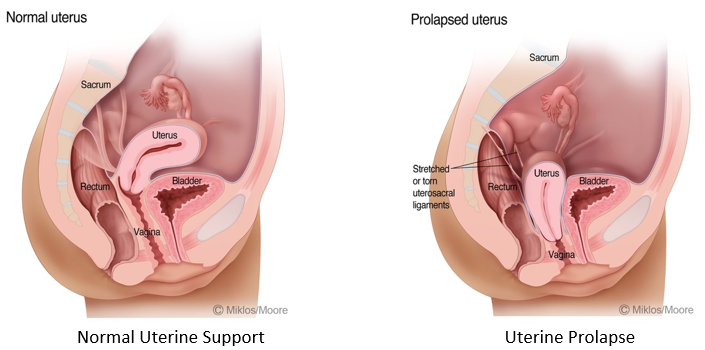
The condition of uterine prolapse is when the uterus falls or descends the vaginal canal when its main supporting ligaments known as the uterosacral ligaments break. This often occurs after trauma to the pelvic floor including: pregnancy, vaginal delivery, injury to the spinal cord or lower back and injury to the nerves that supply the pelvic floor muscles. Though a patient need not have a memorable injury most patients will have had a history of a vaginal delivery.
Signs and symptoms of uterine prolapse include: a bulge at the opening of the vagina or just inside the vaginal opening, lower back discomfort as the day progresses, a feeling of your partner hitting something when engaging in intercourse, pain, pressure, painful intercourse and the inability or difficulty keeping a tampon inside of the vagina during menses. Often a patient can make her own diagnosis by simply using her fingertips to feel the end of the cervix in the lower 1/3 of the vagina.
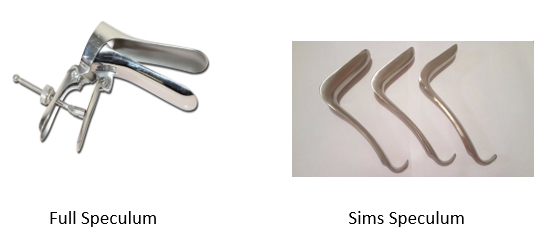
Diagnosis of uterine prolapse requires an experienced physician who examines women for prolapse all the time. The average gynecologist misses the diagnosis of uterine prolapse because they most often use a normal looking speculum which is shaped like a “duck bill”. When a full speculum is placed inside of the vagina the speculum blades pushes the uterus back into position and then the duck bills are opened and this further hide both the ceiling and the floor prolapse defects. It is best to use ½ of a speculum (or a Sims speculum) when examining for any kind of vaginal prolapse (i.e. cystocele, rectocele, urethrocele or enterocele) and especially when evaluating a patient for a uterine or vaginal vault prolapse as this type of speculum will not obscure the prolapse.
Once the diagnosis of uterine prolapse has been made and if the patient is symptomatic i.e. pressure, bulge, pain, painful intercourse. The patient should have the option of treatments.
Treatment Options:
There are several treatment options for uterine prolapse including: pessary supporting devices, kegel exercises (which will never permanently fix the problem), uterine suspension aka hysteropexy and finally a hysterectomy. A hysterectomy is a viable option but should not be offered to a patient as the sole procedure which will fix her prolapse. Yes, it is true that removing the uterus will result in the uterus no longer being prolapsed but the vaginal vault (i.e. the upper 25% of the vagina from which the uterus was removed) will still prolapse. So, if the surgeon just removes the uterus and does not offer concurrent vaginal vault suspension (ie sacrocolpopexy, uterosacral vault suspension, sacrospinous ligaments suspension) the patient will continue to suffer with vaginal vault prolapse.
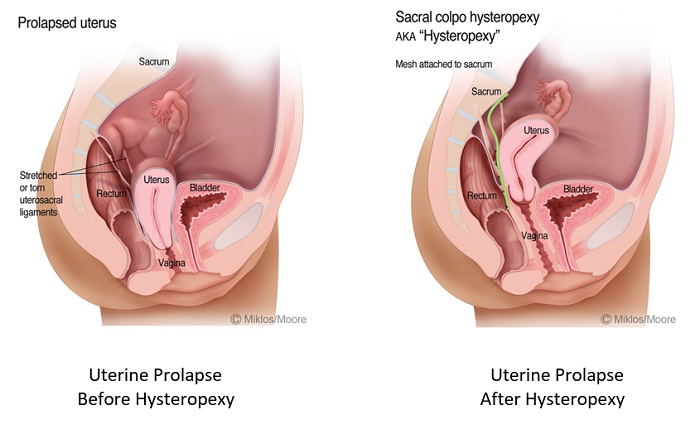
The most successful operation for uterine prolapse while preserving the uterus is the sacrocolpohysteropexy aka hysteropexy. This procedure can be performed with synthetic mesh or with grafts (human, pig or cow). It is well known that human and animal grafts have lower cure rates than the synthetic mesh grafts.
99% of all patients who suffer from a uterine vaginal vault prolapse also have a cystocele and a rectocele and these should be repaired at the same surgery. The key to a successful surgery is choosing a surgeon with a vast amount of experience, expertise and a great reputation.
