Pelvic Pain (adhesions)
Pelvic pain associated with intraabdominal or pelvic adhesions are due to an abnormal fibrous type growth between two structures most often due to trauma or inflammation. Adhesions are also defined as an abnormal cohesiveness between two organ surfaces. The tension and exerted between these two structures results in abdominal or pelvic discomfort. The process of cutting these adhesions is known as adhesiolysis and if the cutting is performed for adhesions specific to the intestines or bowel found in the abdominal or pelvic cavity this type of adhesiolysis is called enterolysis.
Types of Adhesions
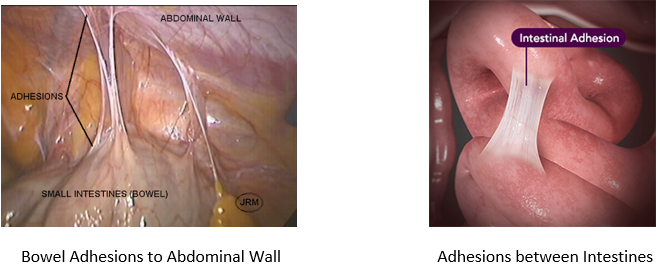
Adhesions are a type of scar tissue that abnormally adhere to different structures. They can be single strands, thin sheets or thick fibrous bands. Adhesions formation is your bodies reaction to damage as it tries to heal itself. Tissue damage can be due to infection, surgery, trauma, radiation therapy or inflammatory disease. Adhesions can occur anywhere but the types of adhesions which cause the most pain are commonly found in the abdominal and pelvic cavity.
Examples of Adhesions:
Incidences
Adhesions are a very common problem especially among patients who suffer from abdominal and pelvic pain. However, they are often ignored for several reasons including many surgeons believe: 1) they do not cause pain, 2) if you cut them they will just return 3) the surgeries can be long and fraught with complications and 4) they are rare and if they are present they are not responsible for the patient’s problems.
However, adhesions are very common and this has been documented in scientific studies including: an autopsy study of which revealed of 752 cadavers 44% had abdominal adhesions (67% of which had prior surgery and 28% who did not have prior abdominal surgery)1 After multiple laparotomies, the incidence of adhesions may even be as high as 93%.2 A systematic review of the literature (2014) revealed that patients had a 54% chance of adhesion formation after abdominal surgery 66% chance after gastrointestinal surgery, 51% chance after obstetrical or gynecologic surgery and 22% after urologic surgery. According to the same study if the patient had her surgery performed by a laparoscopic approach the rate of adhesion formation decreased by 25%.3
Complications
Adhesions do not always mean that a patient will suffer with complications and this is part of the reason that surgeons send a mixed message. Surgeons can see dozens of patients who they identify with intraabdominal or pelvic adhesions and the patients are symptom or complication free. They don’t have any problems so many surgeons do not believe that adhesions cause problems especially pain. However, most surgeons understand adhesions can be responsible for several types of complications including: pelvic and abdominal pain, infertility, and bowel obstruction.
Chronic Pain
In theory, the pain attributed to adhesions is created by both direct tension between two structures with at least one of those structures having sensory nerve endings which is capable of feeling pain and secondly by nerves which sometimes form in grow inside of the actual peritoneal adhesion.4 Although we do not understand the actual function of these peritoneal adhesion nerves one can speculate that they play a role in the development of chronic pain. Cutting adhesions i.e. adhesiolysis does not guarantee a relief of pain however patients have little hope or alternatives to this intervention. What are their choices: 1) do nothing 2) chronic pain control 3) surgery and 4) some have suggested deep tissue massage will help? So, put yourself in the shoes of a patients who is suffering from complications of adhesions especially those who have had previous relief with adhesiolysis. By subjecting themselves to another surgery for adhesiolysis many patients hope they will be afforded at least a few months or years or possibly a lifetime free of pain.
Bowel Obstruction
Adhesions are the number one cause of bowel obstructions in industrialized countries with approximately 1/3 of all cases of obstruction are due to adhesions from a previous surgery. Most bowel obstructions occur within 1-2 years after the pelvic or abdominal surgery thus emphasizing the rapid formation of adhesions and their potential complications.5,6 It has been estimated that approximately 10% of those patients who were treated with adhesiolysis for bowel obstruction will develop a second obstruction emphasizing the recurrence of adhesion reformation.
Other complications:
Other complications associated with pelvic and abdominal adhesions include infertility, urinary urgency and frequency, as well as increase the difficulty of subsequent surgeries which can results in bowel injury, bladder injury, ureteral injury, colostomy and converting a laparoscopy to a laparotomy i.e. large abdominal incision.
Treatment:
The treatment of adhesions via adhesiolysis (aka lysis of adhesions or cutting of adhesions) is the goal of all surgeons who treat the disease. The problem for the patient is there is not a guarantee to whether the adhesions once removed will treat their obstruction, pelvic or abdominal pain, urinary or bowel problems. The only way the patient will ever know is to subject themselves to the surgery. As stated above there is some scientific evidence that supports not doing a laparotomy (large incision) to perform the adhesiolysis but instead using a laparoscopic (small incision approach) as this reduces the reformation of adhesions.
Conclusion:
Adhesions remain a formidable disease as the diagnosis and treatment of the adhesions do not always guarantee patients outcome success. Science and common sense seems to support using the laparoscopic approach over the laparotomy as it may reduce the incidence of adhesion reformation. Adhesion prevention devices, barriers, systemic medications or topical solutions have never been scientifically proven to prevent adhesions but this does not mean they may not work. Future research may one day provide us with a guaranteed anti adhesive barrier but currently that product remains elusive.
|
